Dr Angus Robinson reflects on the EMUC on Urological Cancers 2024
The European Multidisciplinary Congress on Urological Cancers (EMUC) provides a valuable opportunity for practitioners to discuss the latest research and emerging developments in urological cancer treatment and diagnostics. We sponsored Consultant Clinical Oncologist Dr Angus Robinson to attend the conference and, after the event, he shared his insight and reflections with us.
I was delighted to attend EMUC again this year. The event is different to other meetings in that it successfully brings together a wide range of clinicians including surgeons, radiologists and oncologists as well as researchers and other health care professionals, who are all focused on improving outcomes for patients with urological cancers. From the evolving debate around cancer screening to understanding emerging treatments, the congress is an opportunity to evaluate the progress being made across Europe and share our thoughts on the challenges that lie ahead.
The value and challenges of prostate cancer screening
One of the most engaging discussions this year revolved around screening programmes for prostate cancer, an area where opinion remains divided. While it’s clear that early detection is key to improving survival rates, the complexity of implementing an effective screening programme is a recurring theme. We explored the potential benefits of PSA (prostate-specific antigen) testing, alongside newer developments with MRI scanning in those patients with a raised PSA – something that has undoubtedly changed the landscape since previous prostate cancer screening trials.
However, the pitfalls of overdiagnosis and overtreatment were also discussed extensively. Many of us shared concerns about subjecting patients to unnecessary biopsies and treatments for cancers that may never cause harm.
Diagnosis of the disease has increased dramatically since the 1980s but mortality hasn’t followed suit. In the UK, the recent media coverage of Sir Chris Hoy’s diagnosis has raised further awareness and drive more people to report their prostate cancer symptoms and ask for PSA testing. However, the challenge in implementing a nationwide screening programme is in striking the right balance.
The key aim is to identify those patients with important disease and diagnose their cancers at an early stage , but there also needs to be away to limit the physical and psychological burden of diagnosing and treating asymptomatic low risk cancers that are unlikely to impact a patient’s health or natural lifespan. This is an area that will require continued discussion and analysis.

Diagnosis and management of advanced cancers
On the therapeutic front, there was considerable optimism about the advances in diagnostics and combined therapies. A key topic was the role of imaging, particularly PSMA PET scans (positron emission tomography), in the staging of prostate cancer. PSMA PET scans in particular have recently gained traction as a huge advance, especially in detecting metastatic disease in prostate cancers. The potential of PET scans in improving early detection and guiding treatment is promising, especially when combined with other imaging techniques such as CT and MRI. However, accessibility and cost remain barriers to widespread use in public health systems such as the NHS.
Another major area of focus at the congress was radiotherapy, particularly its role in managing localised and advanced urological cancers. The refinement of radiotherapy techniques has significantly improved precision, enabling higher doses of radiation to be delivered with minimal damage to surrounding healthy tissues. For prostate cancer, radiotherapy is now considered an equally viable option to surgery for many patients even in the context of advanced metastatic disease – known as stereotactic radiotherapy in oligometastatic disease.
What’s next?
This year’s EMUC once again underscored both the remarkable progress we’ve made in urological cancer treatment and the work that remains. The congress always inspires a sense of optimism and drive for further research as well as belief that working together as a multidisciplinary community there are many opportunities to tackle these complex challenges.
In terms of everyday practice, being able to answer patients’ questions about the latest treatment and diagnostic developments is a huge benefit of attending the event. As an oncologist, it’s vital to stay updated on changes to best practices and advancements in urological cancer treatment and diagnostics to ensure we provide our patients with the very best care.

About Sciensus
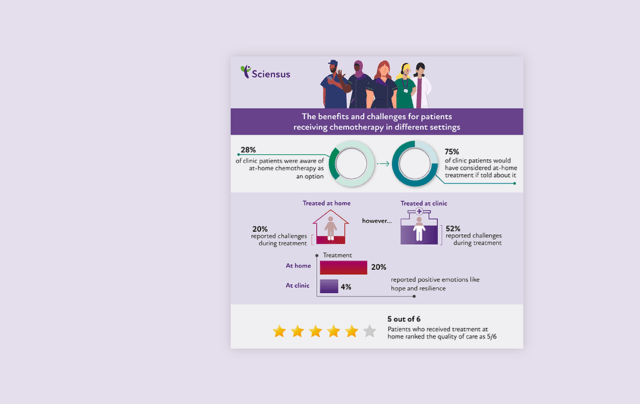
At Sciensus, we believe that making patients’ experience of cancer treatment as straightforward and supportive as possible can improve their overall experience and outcomes. Key to this is offering more choice to patients, whether that’s over the form of treatment they receive or where they receive it.
To find out more, visit our cancer services page.
Read more on…

Blogs
Highlights from the ESMO 2024 conference
The recent 2024 European Society for Medical Oncology (ESMO) congress held in Barcelona was a focus for discussing and displaying…
Blogs
Benefits in receiving chemotherapy at home vs the clinic
An independent exploration of the patient benefits of home cancer treatment. Discover the benefits of home cancer treatment from Sciensus’…

Blogs
Head and Neck Cancer: Insights into an overlooked disease
Head and neck cancers, though less well-known than other types of cancer, represent a significant health challenge in the UK…